Dietitian Shares: Do breastfeeding mothers need probiotics supplements?
Probiotics are beneficial bacteria that can help promote a healthy gut and immune system. Apart from the constant enquiry on foods to boost milk supply, there has been so much rave about probiotics and its supposed benefits to “boost your immune system”. Technically, an optimal functioning immune system is more ideal rather than a boosted immune system that may be overworking and be on overdrive.
Probiotics supplements are currently not known as a drug but as a supplement. Many claims that it is safe and would not pose any health risk to children or mothers. The reality is, there aren’t adequate studies on the safety of long term probiotic supplement intake in children, breastfeeding women or pregnant women. There isn’t enough studies on how it may affect children in the long term if they are taking it as an infant.
It’s also worth noting that probiotics can also be obtained naturally from fermented foods. An optimal gut microbiome is formed from eating a diet rich in pro and prebiotic rich foods such as yogurt, kefir, sauerkraut, kimchi, other fermented foods, fruits and vegetables are a safe and natural way to get probiotics.
There are several possible benefits and cautionary points to consider before taking unprescribed probiotic supplements from the shelves.
Possible Mucosal infection in infants
Mucosal infections included oral, respiratory and gastrointestinal infections. Interestingly, a study found that infants that had the first 6 months of life supplemented with probiotics via maternal intake had higher rates of mucosal infection in the first 2 years of life compared to the no probiotics supplementation group. Despite probiotics seemingly not having any differences on the presence of antibodies in mother’s breast milk among the two groups, there was a modest increase in antibodies in infant’s stools at 5 months of age in the probiotics exposed group as compared to the group not exposed to probiotics.
It is generally known that the colonizers of the infant’s gut would eventually have Bifidobacterium present after a week . In those that are exposed to probiotics, infants had higher Bifidobacterium in their stool less than 1 week, suggesting that probiotics may be promoting earlier colonization of the Bifidobacterium which increases the sIgA in stools too.
This correlative evidence suggests that early probiotic exposure may influence the normal development of the infant’s immune system. Thus there should be some caution in using probiotics. If taken should be monitored by a doctor accordingly and not taken carelessly off the counter.
Effective for mastitis?
There is definitely a group of mothers who experience breast engorgement due to hyperlactation which is less talked about. This group of mothers are at higher risk of experiencing mastitis and finding foods to increase breast milk is probably the last thing on their minds. Increasing breast milk food is not their priority
Acute mastitis is one of the leading causes of why breastfeeding women stop breastfeeding. 1 in every 4 women may have acute mastitis during the first 26 weeks of postpartum. It is common to use antibiotics as clinical treatment when mothers do suffer from mastitis. However, there are growing concerns on the exposure of antibiotics to infants at such a young age and potentially affecting the microbial content of breast milk and developing antibiotics resistance in infants and mothers. Although narrow spectrum antibiotics are recommended to treat the pathogen specific causing mastitis to minimize this risk, broad spectrum antibiotics are still commonly used. Thus, finding scientifically effective and safe alternatives to treating and preventing mastitis in breastfeeding women has been a growing trend.
Some may claim that probiotic supplements may help to reduce risk of mastitis. However, available studies showed mixed results with mastitis in cows. So far, there is only one trial in breastfeeding women and its efficacy has not been established. Based on a systematic study in 2022, duration and effective strategies of supplementation have not been established either.
Preventative from developing allergy
The American Academy of Pediatrics, European Academy of Allergy and Clinical Immunology and the National Institute of Allergy and Infectious Diseases do not recommend probiotics as the primary prevention of allergic diseases. The main recommendation is to expose the 9 allergenic foods as early as during pregnancy and breastfeeding through the mother’s dietary intake in order for the fetus to develop an immune tolerance towards such foods. Early exposure helps to reduce the risk of developing food allergies later in childhood.
The World Allergy Organization (WAO) is more in favour of supplementation during and after pregnancy in mothers who have a history of allergy in the family. However it is not based on the efficacy of probiotics on preventing allergy but more on the basis of “unlikely to harm”. It is important to note that till to this date, there isn’t a specific probiotic strain that is found to be effective. Previous studies used the same species of probiotics but not the same specific strain.
Conclusion
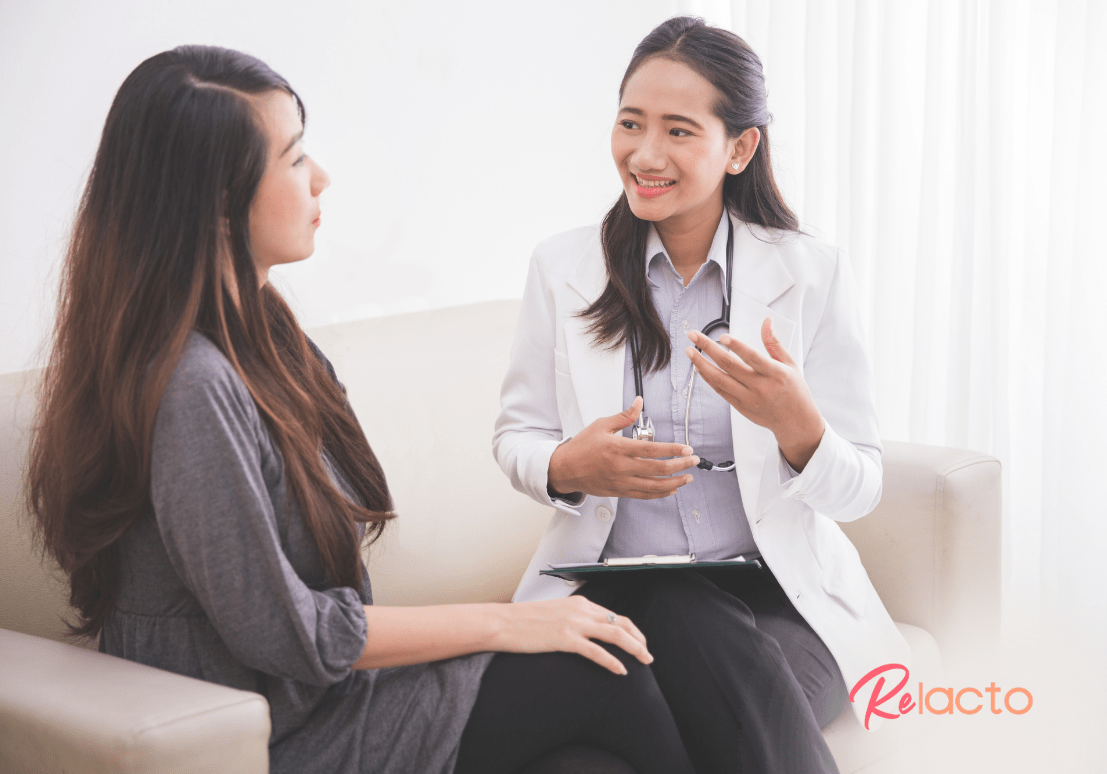
In summary, there are several possible benefits of taking probiotics however there should be more caution around taking these probiotics supplements. Discuss with your doctor or dietitian before taking. Only taken when necessary and under the supervision of your doctors or dietitian.
A healthy gut with a diverse microbiome that supports an optimal functioning immune system comes first and foremost from a diet that has a wide variety of plant based food ingredients from vegetables, fruits, wholegrains, legumes, beans, traditional fermented foods and vegetable oils.
Such a diet should be your main priority and foundation as it will be more bullet proof in supporting your overall health. Supplements should stay as something supplementary, not something that cures all and treats all.
Speak to a dietitian or a doctor who has an expertise in the area so that you can obtain more personalized advice if you are considering taking probiotics supplements during pregnancy or breastfeeding.